NeuroRehabilitation
SPECS has advanced the Rehabilitation Gaming System (RGS), a new brain theory-based tool for the rehabilitation of deficits due to brain lesions.
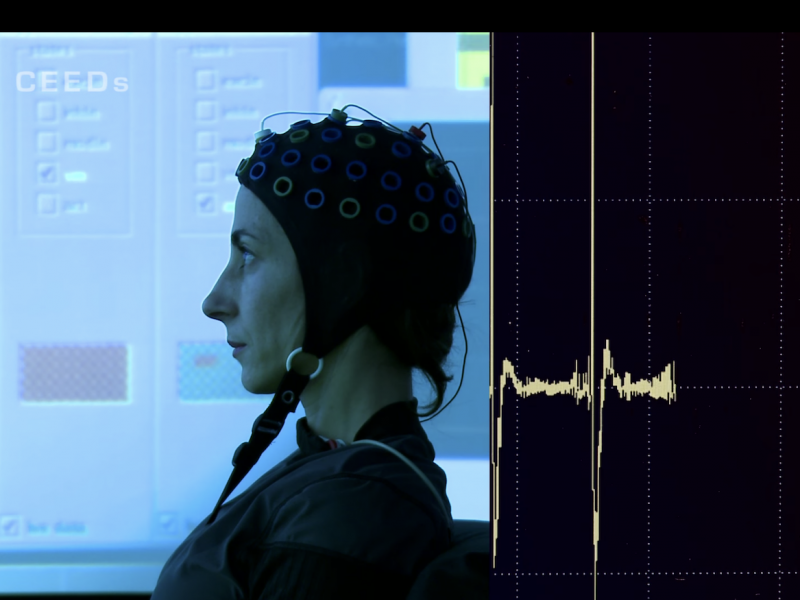
RGS is a Virtual Reality-based technology for neurorehabilitation after brain damage and is based on neuroscientific principles of brain plasticity, motor and cognitive learning in health and disease. The clinical benefit of the system have been studied in acute, sub-acute and chronic stroke patients, both at the clinic and in the domiciliary context (Ballester, et al., 2017, Cameirao 2010).

Stroke can cause brain damage with loss of motor and cognitive functions.

A stroke patient training with RGS (Val d’Hebron Hospital in Barcelona).
The RGS platform

Principles of NeuroRehabilitation
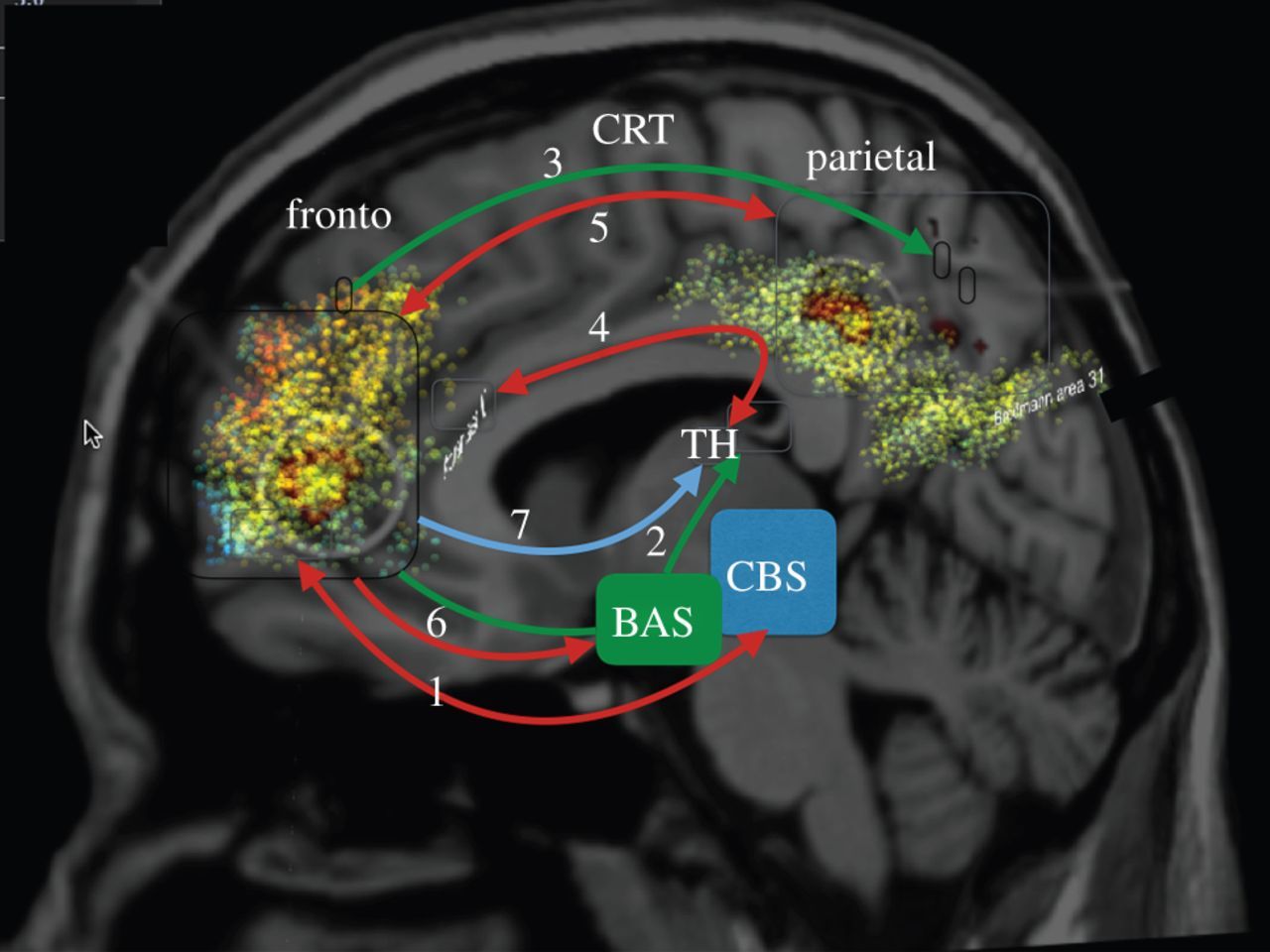
The motivation behind the development of a neurorehabilitation system such as RGS was driven by the intuition that combining interaction technology, in particular, virtual reality, with the DAC theory of mind and brain would make an impact on the recovery of brain function at the clinical level. This decision was a key step in the realization of RGS since it made choices on the content of non-arbitrary treatment protocols and every intervention became a well-defined interaction with a user, which in turn would provide immediate feedback on the system in terms of its usability, and effectiveness. RGS is based on the neurobiological considerations that plasticity of the brain remains throughout life and therefore can be utilized to achieve functional reorganization of the brain areas affected by stroke.
By now RGS incorporates about 20 specific DAC derived principles that range from the key role of sensori-motor contingencies in organizing cognition and action (see Prochnow, D. et al., Eur. J. of Neurosc. 2013) to the importance of goal-oriented and error-driven intervention. (see Belen Rubio Ballester et al., J. NeuroEng. Rehab. 2015)
In the last five years, SPECS has discovered new principles of rehabilitation derived from its theoretical neuroscience agenda.
– For instance, we have shown that functional recovery depends on the minimization of perceived error as opposed to physical error (Rubio et al. 2015), a direct confirmation and application of the counterfactual error learning model.
– Further, we have found definite proof for distinct cortical reorganization resulting from RGS rehabilitation that strongly correlates with functional recovery (Rubio et al. 2017), clinically successfully validated an RGS aphasia rehabilitation protocol (Grechuta et al., 2016, 2017, In press Stroke).
We this we have also resolved a controversy that has hampered the field on the effectivity of virtual reality as an intervention method. In two meta-analyses published shortly, we have shown first that the core issue is one of the principles, not technology, in particular, the cognitive approach advanced by RGS (Maier et al., 2019, NRR). Secondly, that as opposed to the presence of a rather short critical time window of plasticity serving recovery, RGS sees an expanded decaying level of plasticity of up to three years (Rubio et al., In Press, J Neurophys.). SPECS is in a unique position to perform these analyses because of the large number of clinical trials we have realized working with the main hospitals in Barcelona and beyond.
Clinical validation
To support the clinical validation we have installed RGS neurorehabilitation-stations in several hospitals. As a result, RGS has built up an unprecedented empirical track record (see references) having been tested with over 1500 patients at the acute and chronic stages of stroke, including at home settings. In comparison to occupational therapy, RGS has shown a positive impact in functional and structural recovery as captured by standardized clinical scales. (M. S. Cameirao, et al., 2011)

Further, in more recent studies, an extended version of the RGS protocol that includes implicit reinforcement mechanisms for action selection has shown positive effects on the amount of use of the more affected arm (Ballester, et al., 2015), these changes in limb use were associated with sustained functional gains (Ballester, et al., 2016).
Building on these results, together with our clinical partners, we are now validating the generalization of RGS to other neuropathologies such as Cerebral Palsy, Traumatic Brain Injury, and Aphasia.
Collaboration with the clinic
To support the clinical studies we have installed RGS training-stations in several hospitals. As a result, RGS has built up an unprecedented empirical track record (see key references) having been tested with over 1500 patients at the acute and chronic stages of stroke, including at home settings. Building on these results, together with our clinical partners, we are now validating the generalization of RGS to other neuropathologies such as Cerebral Palsy, Traumatic Brain Injury, and Aphasia.
- Hospital Universitari de la Vall d’Hebron (HUVH)
- Parc Salut de Mar
- Hospital del Mar i de l’Esperança
- Heinrich Heine Universität
- Fundació Tic Salut
- Institut Municipal d’Assistència Sanitària (IMAS)
- Hospital Clinic
(see also AAL project http://rgs-project.upf.edu/home and project SANaR http://sanar.project.upf.edu/)
RGS impact
“Stroke patients want to continue using RGS after participating in clinical trials”
RGS has been validated with over 1500 patients and is introduced in the market through the spin-off company Eodyne. RGS has an EC certification.
This demand combined with the clinical results show that RGS is more effective than any other intervention available today has led us to the creation of the spin-off company Eodyne.com.
Eodyne’s goal is to make RGS available to as many people as possible for a minimum cost.
Publications
A Wearable Device to Overcome Post-Stroke Learned Non-Use. Methodology, Design and Usability of the Rehabilitation Gaming System for wearables. De la Torre Costa J., Ballester B.R., Verschure P.F.M.J. IC-IHAW 2021 Conference. 8-9 November 2021.
Caballeria, E., Maier, M., Balcells-Oliveró, M., López-Pelayo, H., Oliveras, C., Rubio Ballester, B., … & Gual, A. (2021). Rehabilitation Gaming System for Alcohol-Related Cognitive Impairment: A Pilot Usability Study. Alcohol and Alcoholism. https://doi.org/10.1093/alcalc/agab043
Ballester, B. R., Ward, N. S., Brander, F., Maier, M., Kelly, K., & Verschure, P. F. (2021). Relationship between intensity and recovery in post-stroke rehabilitation: a retrospective analysis. Journal of Neurology, Neurosurgery & Psychiatry. http://dx.doi.org/10.1136/jnnp-2021-326948
Grechuta, K., Ballester, B. R., Munné, R. E., Bernal, T. U., Hervás, B. M., Mohr, B., … & Verschure, P. F. (2020). Multisensory cueing facilitates naming in aphasia.
Wiers, R. W., & Verschure, P. (2020). Curing the Broken Brain Model of Addiction: Neurorehabilitation from a Systems Perspective. Addictive Behaviors, 106602. https://doi.org/10.1016/j.addbeh.2020.106602
López-Carral H, Grechuta K, Verschure PFMJ (2020). Subjective ratings of emotive stimuli predict the impact of the COVID-19 quarantine on affective states. PLoS ONE 15(8): e0237631. https://doi.org/10.1371/journal.pone.0237631
Maier, M., Ballester, B. R., Bañuelos, N. L., Oller, E. D., & Verschure, P. F. (2020). Adaptive conjunctive cognitive training (ACCT) in virtual reality for chronic stroke patients: a randomized controlled pilot trial. Journal of NeuroEngineering and Rehabilitation, 17(1), 1-20.
Grechuta, K., Rubio Ballester, B., Espín Munne, R., Usabiaga Bernal, T., Molina Hervás, B., Mohr, B., … & Verschure, P. (2019). Augmented Dyadic Therapy Boosts Recovery of Language Function in Patients With Nonfluent Aphasia: A Randomized Controlled Trial. Stroke, 50:1270–1274. – https://www.ahajournals.org/doi/10.1161/STROKEAHA.118.023729
Grechuta, K., Ulysse, L., Rubio Ballester, B., & Verschure, P. (2019). Self beyond the body: action-driven and task-relevant purely distal cues modulate performance and body ownership. Frontiers in Human Neuroscience, 13, 91.
Maier, M., Rubio Ballester, B., Duff, A., Duarte Oller, E., & Verschure, P. F. (2019). Effect of Specific Over Nonspecific VR-Based Rehabilitation on Poststroke Motor Recovery: A Systematic Meta-analysis. Neurorehabilitation and Neural Repair. https://doi.org/10.1177/1545968318820169
Ballester, B. R., Duff, A., Maier, M., Cameirao, M., Bermudez, S., Duarte, E., … & Verschure, P. F. (2018). Revealing an extended critical window of recovery post-stroke. bioRxiv, 458745.
Ballester, B. R., Grechuta, K., Maier, M., & Verschure, P. F. M. (2018, January). Extending the proportional recovery rule to virtual reality-based neurorehabilitation. In Cerebrovascular diseases (vol. 45, pp. 417-417). Allschwilerstrasse 10, ch-4009 Basel, Switzerland: Karger.
Maier, M., Bañuelos, N. L., Ballester, B. R., Duarte, E., & Verschure, P. F. (2017, July). Conjunctive rehabilitation of multiple cognitive domains for chronic stroke patients in virtual reality. In Rehabilitation Robotics (ICORR), 2017 International Conference on (pp. 947-952). IEEE.
Grechuta, K., Guga, J., Maffei, G., Ballester, B. R., & Verschure, P. F. (2017). Visuotactile integration modulates motor performance in a perceptual decision-making task. Scientific reports, 7(1), 3333.
Ballester, B. R., Nirme, J., Camacho, I., Duarte, E., Rodríguez, S., Cuxart, A., … & Verschure, P. F. (2017). Domiciliary VR-Based Therapy for Functional Recovery and Cortical Reorganization: Randomized Controlled Trial in Participants at the Chronic Stage Post Stroke. JMIR serious games, 5(3), e15-e15.
Belén Rubio Ballester, Martina Maier, Rosa María San Segundo Mozo, Victoria Castañeda, Armin Duff and Paul F. M. J. Verschure (2016), “Counteracting learned non-use in chronic stroke patients with reinforcement-induced movement therapy”. Journal of NeuroEngineering and Rehabilitation. DOI: 10.1186/s12984-016-0178-x
Belén Rubio Ballester, Jens Nirme, Esther Duarte, Ampar Cuxart, Susana Rodriguez, Paul Verschure and Armin Duff (2015), “The visual amplification of goal-oriented movements counteracts acquired non-use in hemiparetic stroke patients”. Journal of NeuroEngineering and Rehabilitation, 12:50 ; doi 10.1186/s12984-015-0039-z.
Maier, M., Rubio Ballester, B., Duarte, E., Duff, A. and Verschure, Paul F.M.J. (2014). “Social Integration of Stroke Patients through the Multiplayer Rehabilitation Gaming System“. Games for Training, Education, Health and Sports. Lecture Notes in Computer Science Volume 8395, 2014, pp 100-114.
Nirme, J., Duff A., & Verschure P.F.M.J. (2012) “Adaptive Enhanced Mapping Of Upper Limb Movement In A Virtual Reality System For Stroke Rehabilitation”. Conference Abstract presented at the 8th FENS Forum of Neuroscience, Barcelona, Spain.
Duff, A. (2012). Non-immersive virtual reality and motoric neurorehabilitation: Rehabilitation Gaming System. Acta Clin Croat, 51(2).
Mónica S. Cameirão, Sergi Bermúdez i Badia, Esther Duarte, Antonio Frisoli, and Paul F.M.J. Verschure. The combined impact of Virtual Reality Neurorehabilitation and its interfaces on upper extremity functional recovery in patients with chronic stroke. “Stroke”, vol. 43 (10) 2720-2728, 2012
Rodriguez, S., Bermudez i Badia, S., Cameirão, M. S., Fina, A. C., Duarte, E., Duff, A., Verschure, P. F. M. J., et al. (2011). “Effects of Virtual Reality Upper Limb Based Training (Rehabilitation Gaming System) on Spasticity, Shoulder Pain, and Depression After Stroke”. 2011 AAPM&R annual assembly (Vol. 3, p. S160). Elsevier Inc. doi:10.1016/j.pmrj.2011.08.013.
Verschure, P. F. M. J. (2011). “Neuroscience, virtual reality and neurorehabilitation: brain repair as a validation of brain theory”. Conference proceedings for the Annual International Conference of the IEEE Engineering in Medicine and Biology Society. IEEE Engineering in Medicine and Biology Society. (Vol. 2011, pp. 2254–7). IEEE.
Nirme, J., A. Duff, and P.F.M.J. Verschure. “Adaptive rehabilitation gaming system: On-line individualization of stroke rehabilitation”. in Engineering in Medicine and Biology Society, EMBC, 2011 Annual International Conference of the IEEE. 2011. IEEE.
Duff, A., Duarte, E., Cuxart, A., Rodríguez, S., Cameirão, M., i Badia, B. S., & Verschure, P. (2011). Rehabilitation Gaming System (rgs): The Impact Of Virtual Reality Based Training On Upper Limb Recovery In The Acute And Chronic Phase Of Stroke. Cerebrovascular Diseases, 31, 190.
M. S. Cameirao, et al., “Virtual reality based rehabilitation speeds up functional recovery of the upper extremities after stroke: A randomized controlled pilot study in the acute phase of stroke using the Rehabilitation Gaming System“, Restor Neurol Neurosci, vol. 29, pp. 287-98, 2011
M. S. Cameirao, et al., “Neurorehabilitation using the virtual reality based Rehabilitation Gaming System: methodology, design, psychometrics, usability and validation“, J Neuroeng Rehabil, vol. 7, p. 48, 2010.
Cameirao, M. S., Bermúdez, I. B. S., Duarte Oller, E., & Verschure, P. F. (2009). The rehabilitation gaming system: a review. Stud Health Technol Inform, 145(6).
Cameirão, M. S., Badia, S. B., Oller, E. D., & Verschure, P. F. (2008). Stroke Rehabilitation using the Rehabilitation Gaming System (RGS): Initial Results of a Clinical Study. Annual Review of CyberTherapy and Telemedicine, 146.
Cameirão, M. S., i Badia, S. B., Zimmerli, L., Oller, E. D., & Verschure, P. F. (2007, September). The rehabilitation gaming system: a virtual reality based system for the evaluation and rehabilitation of motor deficits. In Virtual Rehabilitation, 2007 (pp. 29-33). IEEE.
Cameirão, M. S., Badia, S. B. I., Zimmerli, L., Oller, E. D., & Verschure, P. F. M. J. (2007). A virtual reality system for motor and cognitive neurorehabilitation.
Cameirão, M. S., i Badia, S. B., Mayank, K., Guger, C., & Verschure, P. F. M. J. (2007). Physiological responses during performance within a virtual scenario for the rehabilitation of motor deficits. PRESENCE 2007.